More On Cervical Cancer/Pap Tests
More On Cervical Cancer/Pap TestsAnswered by Dr. Chris Awtrey, Division of Gynecologic Oncology, Beth Israel Deaconess Medical Center and Dr. Hope Ricciotti, Obstetrician/Gynecologist, The Dimock Center.
Q: What is cervical cancer?The cervix is the lowest part of the uterus (womb) and connects it to the upper vaginal canal. Cancers of the cervix generally develop from the lowest portion where the uterus and the vaginal canal meet. Cancers are either described as squamous, which are similar to skin cells or glandular (adenocarcinoma) which are similar to mucus secreting cells of the gastrointestinal tract. In the United States there are estimated to be over 11,000 cases diagnosed in 2007 and 3,670 women will die of the disease. Cervical cancers do not develop quickly from normal cervical cells but gradually go through a progression from a precancerous state to cancer, a process which occurs as a result of exposure to the human papillomavirus (HPV). Thankfully, only a fraction of patients with precancers of the cervix, a condition known as cervical dysplasia, develop cancer.
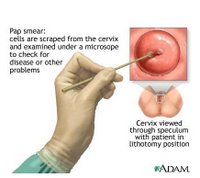
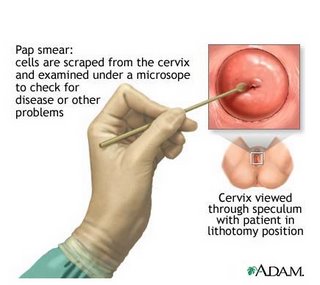
Q: Can cervical cancer be prevented? How?There are two ways to prevent cervical cancer. The first is to avoid exposure to the human papillomavirus (HPV) either by not engaging in intercourse or limiting the number of partners. Condom use also reduces the risk of getting HPV. Another good way of preventing the disease is to be vaccinated to the subtypes of HPV known to cause 70% of the precancerous condition (dysplasia) and the cancer. The HPV vaccine Guardasil is now available for women 26 and under. Because cancer of the cervix generally develops slowly and progresses through a precancerous state known as dysplasia, identifying and treating precancerous changes through the use of pap testing cervical is the other way to prevent cervical cancer. Cells from the cervix can be sampled at time of pelvic exam using a pap test, which can identify precancerous cells of the cervix.
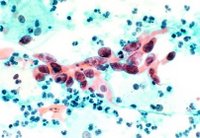
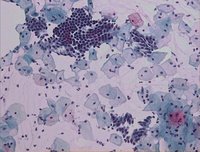
Q: How do you screen for cervical cancer?Screening for cervical cancer is performed at the time of annual pelvic exam by using a pap test. We can sample some of the cells of the ectocervix, where these cancers generally develop and identify precancerous microscopically. This is how we identify a change before a real cancer develops. The biology of cervical cancer is that it happens to have a long (many years) precancerous phase, and that is why cervical cancer screening has been so successful
Q: What exactly is a Pap test?A Pap test is a sampling of the cells of the cervix using a brush or small, narrow scraping paddle. It is the most effective cancer screening tool that physicians have to prevent cancer. Sampling does not harm the cervix and for women having a pelvic exam the sampling is generally not a painful process and is well tolerated. Since we have been using Pap tests, the incidence of cervical cancer has dropped dramatically. Now, with the HPV vaccine, it should go even lower.
Q: Who should get a Pap test and how often?The general rule is that women who are sexually active or have been in the past should be screened for cervical cancer starting three years after the onset of sexually activity, or by age 21, on a yearly basis. Once a woman has a series of normal pap tests for three straight years, this testing interval can be increased. However, this should only be done after consulting with your health care provider.
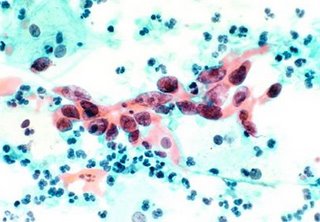
Q: What is the liquid-based Pap test?Pap tests originally were performed by smearing the cells removed from the ectocervix on a glass slide. Recent innovations have revolutionized the old pap smear and now practitioners in the U.S. generally use the new liquid-based test. This essentially replaces the glass slide. Now, the cells are taken from the brush and floated into a liquid preservative. This allows for less clumping of the cells on a slide and removes debris and mucus from the sample, which made the old pap smears harder to read. Data on this new liquid-based technology shows that it reduces the number of tests needed to be repeated due to unclear sampling and may even increase the pick-up rate of cancers and precancers. HPV testing is also done as part of the liquid pap test, which adds to our ability to decide which pap test results need treatment.
Q: Are cervical cancer vaccines approved by the FDA?Cervical cancer vaccines are vaccines against the HPV virus sub-types that are associated with development of cervical dysplasia and cancers. The vaccine Guardasil is FDA-approved and is given as a series of three injections over six months, and ideally should be given to women prior to potential exposure to HPV, for example, before starting to have sexual intercourse. So it is currently recommended for young girls ages 9-11. However, it is FDA approved through age 26, and we are therefore doing “catch up” vaccines for young women to get them vaccinated.
Q: Who should receive the vaccine?At this point the American Cancer Society recommends that the vaccine be given to girls age 11-12 and as early as age 9, at the discretion of a pediatrician. Older women up to age 26 should be counseled on receiving vaccination and are eligible to have catch-up vaccination. It is unclear if women older than 26 benefit from the vaccine. There is another vaccine awaiting FDA approval that will have a higher age cut-off.
Q: What is the age cut-off for receiving the vaccine?At this point, the cut-off for receiving the vaccine is 26. Insurance will not cover the cost of the vaccine if you are older than 26.
Labels: Cervical Cancer Awareness, Cervical Cancer Prevention, Pap Smear Test