Ann Arbor, MI
She wants to shop for a prom dress, buy clothing at a regular mall store and walk easily across the stage on graduation day.
"I don't want to wheeze when I grab my diploma," said Sarah White, 16, of Vandercook Lake. "I don't want to graduate in a really large gown."
With more than 410 pounds on her 5-foot, 4-inch frame, the Vandercook Lake High School junior is desperate to lose the weight that for years has restricted her activities, drawn sneers from some classmates and compromised her health.
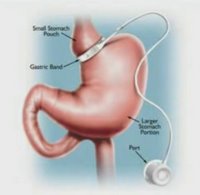
About gastric bypass surgery
The surgery changes the anatomy of a patient's digestive system to limit the amount of food that can be eaten and digested. It redirects food to bypass most of the stomach and flow directly into the middle of the small intestine, which limits calorie absorption. The surgeon uses staples to create a walnut-sized pouch at the top of the stomach that holds about an ounce of food and sews part of the small intestine directly onto the pouch. Risks include death, blood clots in the legs, leaking at the staple lines in the stomach and dumping syndrome, caused by stomach contents moving too quickly through the small intestine. The syndrome causes diarrhea, abdominal cramps, vomiting, sweating and dizziness.
— Source: Mayo �Foundation for Medical Education and Research
She is scheduled to undergo gastric bypass surgery Tuesday at C.S. Mott Children's Hospital at the University of Michigan in Ann Arbor. White will be the first adolescent to have the weight-loss surgery as part of the UM Health System's new Pediatric Comprehensive Weight Management Center program.
"Her health is so significantly affected that surgery is warranted," said Dr. Susan Woolford, a university pediatrician and the center's medical director.
The university set up the family-focused program a year ago to combat the growing problem of childhood obesity. White entered in February 2007 when she was at her peak weight of 423 pounds, said her mother, Patricia White.
Sarah White revamped her diet and started exercising more, but did not lose much weight due to underlying health conditions, including a thyroid problem, Woolford said.
The surgery, which restructures the digestive tract and shrinks the stomach to limit the intake of food, is becoming increasingly common among teens as more struggle with obesity. But it still is not performed often, doctors said.
Some children's hospitals do not offer the surgery, and Woolford said she doesn't know of gastric bypass ever having been performed on an adolescent at UM.
According to medical literature, there are concerns about the long-term effects and the ability of pediatric patients to give informed consent to an invasive procedure that involves a lifetime of follow-up care and dietary restrictions.
"I had no other option," said White, who with support from her mother made the decision to go ahead with the procedure despite some early reservations.
"I was scared about all my intestines looking like a modern-day Picasso," she said Friday at the high school. She plays clarinet in the band, belongs to Students Against Destructive Decisions and said she has a 3.79 grade point average.
She had some qualms about the permanency of the surgery, "But it's either face up to eternity or die at 20," she said.
Fighting the weight
For years, White's weight-loss attempts have failed.
"I remember in elementary school, she bought salads and white milk or water when she bought lunch every day; that didn't work. She walked three miles a day and that didn't work," said her friend, Kelsey Weathers, 16, a diminutive girl who has been friends with White since kindergarten.
White once joined Weight Watchers with her grandmother, but said it seemed weird to be with a group of older women. She didn't lose weight, became frustrated and quit.
She weighed 6 pounds, 13 ounces at birth but quickly gained weight, developing faster than average children, her mother said.
Sometimes it is just easier and cheaper to eat at McDonald's than buy healthier foods, said Sarah White, who listed her weaknesses as Mexican food and pizza. At times, she struggled with emotional eating, but wasn't the type who raided the refrigerator at night, her mother said.
"Her body just doesn't metabolize the food," Patricia White said of her daughter, who was diagnosed at an early age with a type of hypothyroidism, meaning her thyroid gland doesn't produce enough of certain hormones, which impact metabolism.
By Dave Weatherwax | Jackson Citizen PatriotSarah White collapses her head on her mother's shoulder, Patricia White, after finishing her workout Friday afternoon at Planet Fitness of Jackson.
Both sides of her family have overweight members, said Patricia White, whose brother had gastric bypass surgery about two years ago. "She is genetically screwed."
Her daughter was obese by age 8, said White, a single, working mother who is both fiercely protective and proud of her daughter.
The two are clearly close and tease each other continually.
Friday, Patricia White razzed her daughter about her weight-induced spinal curvature, calling her Quasimodo.
"Well, he got the girl in the end, so there is hope for me," Sarah White countered, smiling.
Struggling with pain
The surgery is expected fix some of her problems, such as the curvature and the weight-related pain she feels in her back and knees.
At 8, Sarah White was diagnosed with type 2 diabetes and metabolic syndrome, a cluster of conditions that occur together and increase risk of heart disease, stroke and diabetes.
The excess weight has affected her self-esteem, her friends said. She regularly endures strangers' stares. It also makes school occasionally difficult.
Though White is witty, reads regularly and impresses friends with her vocabulary, her classmates haven't always been accepting, she said. "Especially in middle school, when everyone is discovering the opposite sex."
She cried often then.
Before she got involved with the program at UM Health System, which taught her to change some of the behaviors that contributed to her weight issues, she said she felt like a panda.
"All I did was sit around and eat and look cute," said White, who likes pandas and has many stuffed versions of them in her oriental-themed bedroom.
By the time she got to high school, things got better as the focus turned to academics.
More info
For more information about the University of Michigan's Pediatric Comprehensive Weight Management Center, visit www.med.umich.edu/MPOWER
"I've always been the smart fat kid, which is better than just being the fat kid," said White, who speaks openly and often comically about her situation.
"What I can't do physically, I make up mentally."
Her band director, Chip Williams, called her a "very good student."
"She is one of my top players," he said after class Friday.
However, White said she cannot both play her clarinet and march because it requires too much air and energy.
Her size keeps her from sitting at classroom desks. Instead, she sits at a table outside the rows other students fill.
For school dances, she has worn a purple pin-stripe suit. "It is hard to be girly in this body," she said.
A new chapter
She is looking forward to shopping for a prom dress after her surgery, which could help her lose 100 pounds by her birthday in January.
Her goal is to lose at least 200 pounds.
The surgery is about 90-percent successful in spurring and maintaining weight loss, said Dr. Henry Buchwald, professor of surgery at the University of Minnesota in Minneapolis, who has specialized in metabolic or bariatric surgery for decades.
The mortality rate in surgery is about 0.5 percent, he said.
Long-term effects of the operation on teens have not entirely been explored because the surgeries have been performed for about 20 years. But the procedures have held up over five-, 10- and 20-year periods, Buchwald said.
"What we hope we are �doing for these adolescents is giving them time. Obesity is �a fatal disease," Buchwald said.
The Tuesday surgery likely will keep White in the hospital for a week and a half, she said.
Her diet will be seriously limited in the weeks after surgery, as it has been in the weeks leading up to surgery.
For lunch Friday, she ate applesauce, a protein shake and yogurt, in compliance with a liquid diet she has been required to follow since Aug. 26.
To avoid temptation, all solid food has been removed from the house, Patricia White said.
After surgery, patients have to stay on course and maintain healthy life style habits to be successful, Woolford said. "Weight-loss surgery is not a magic bullet."
White has made the necessary changes, including incorporating physical activity into her weekly schedule, Woolford said, and has a strong family support structure.
She is rarely, if ever, negative, her friend Weathers said.
Some of the dietary restrictions have been difficult, Sarah and Patricia White said, but the payoff will be worth it.
"It's a small sacrifice to live longer," Patricia White said.
Labels: gastric bypass malpractice lawsuits, patient stories, proper candidate, teen gastric bypass