Knoxville woman undergoes sleeve gastrectomy, very pleased with results

Knoxville, TN
Sara Trombley tried every kind of diet on the market. She did Weight Watchers, liquid diets, and pills. Nothing seemed to help her lose weight and keep it off. She began researching surgery options. She was originally a lap-band patient, but then learned about the gastric sleeve procedure. Sara also says she had to overcome her mental issues in regards to eating.
"I struggled with binge eating disorder for a few years and that's when my weight I almost doubled my weight," she says.
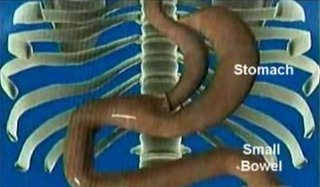
The new procedure is called a sleeve gastrectomy and it involves removing part of the stomach. Dr. Mark Colquitt is one of the first physicians in East Tennessee to perform this new procedure. "You cut the stomach and you remove the bottom half and what's leftover is a sleeve," he explains.
Sara had the surgery in February of 2008 and is very pleased with the results. "I've lost 45 pounds and I couldn't have done that with any diet," she says. "I have confidence that it is going to stay off I'm not constantly scared that if I look at a bag of chips the weight is going to come back on."
Dr. Colquitt says the surgery isn't as risky as gastric bypass but some patients can benefit more than others. "Anybody who meets certain criteria as far as weight generally, you are looking at someone who is 100 pounds overweight. We used a scaled called BMI weight and it has to be 35 or greater."
Sara is pleased with her results since the sleeve procedure but says success starts in the mind. "I think the most important thing is to address any mental emotional issues you have with food. You have to get those taken care of or our not going to be successful for me it's the most important thing."
Labels: patient stories, sleeve gastrectomy