Urologist's opinion: Gastric band placement for obesity is not associated with increased urinary risk of urolithiasis compared to gastric bypass surgery
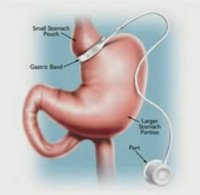
As morbid obesity is becoming increasingly prevalent in our western society, the surgical options for management of this disorder are being more widely utilized. These procedures include Roux-en-Y gastric bypass and gastric band surgery. It has been estimated that the number of bariatric surgeries performed has increased ten-fold in the past decade. It has been observed that in some patients undergoing bariatric surgery for obesity, new onset nephrolithiasis can develop.Gastric Bypass Malpractice Lawsuit Attorneys
These two studies very nicely show that patients at greatest risk are those with Roux-en-Y gastric bypass in which the normal gut flow and absorption is interrupted. These patients typically have an elevation in their urinary oxalate and a significant reduction in their urinary volume. Interestingly, patients with gastric banding appear to have a more significant reduction in their urinary volumes compared to the Roux-en-Y group of patients. However, the Roux-en-Y gastric bypass procedure results in a more significant hyperoxaluria and hypocitraturia.
Both of these studies note that due to the small numbers and the limited time of their study, they were unable to demonstrate that the increased urinary risk factors translated into an actual increased risk for renal stone development. However, it would seem prudent to counsel these patients even before they come to their surgical procedure with regards to dietary modifications to reduce their risk factors for renal stone development. These dietary modifications include maintaining an adequate fluid intake to potentiate a 2-liter urine output per day, 1,200 to 1,500 mg calcium citrate with Vitamin D and 500 mcg Vitamin B-12 and B-complex supplementation. Additional citrate supplementation may be important particularly in those patients with a prior history of stone disease.
Further clinical studies are still required to illustrate the effect of nutrition and pharmacologic therapy on the risk of stone development in patients undergoing bariatric surgery.
Labels: gastric band, gastric bypass research, gastric bypass risks, gastric bypass surgery, gastric bypass surgery alternatives