Wall Street Journal: Study questions cost-effectiveness of Gardasil cervical cancer vaccine
From The Wall Street Journal
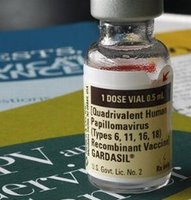
A new study suggests that giving Merck & Co.'s cervical-cancer vaccine Gardasil to women through their mid-20s may not be worth the price, despite U.S. recommendations that this age group receive the costly shot.
The study, published online Wednesday by The New England Journal of Medicine, comes as Merck already is having difficulty persuading college-age and older women to get the vaccine, which was introduced in 2006 and costs about $360 for a three-dose regimen. This has contributed to a slowdown in Gardasil sales, casting a cloud on Merck's financial outlook.
Questions surrounding Gardasil's cost-effectiveness also could make for tougher market conditions for GlaxoSmithKline PLC's Cervarix, a cervical-cancer vaccine that is available outside the U.S. and is under review by the U.S. Food and Drug Administration.
Gardasil is designed to prevent infection by four strains of the human papillomavirus, or HPV, which is transmitted through sexual activity. Two of the targeted HPV strains are believed to cause about 70% of all cervical-cancer cases, while the other targeted strains cause most cases of genital warts. HPV also can cause other, rare tumor types such as vaginal and anal cancers. Gardasil isn't guaranteed to prevent cervical cancer because it doesn't protect against certain cancer-causing HPV strains.
The FDA approved Gardasil for use in females ages 9 to 26. The Centers for Disease Control and Prevention recommends routine HPV vaccination for girls 11 and 12 years old, as well as a temporary "catchup" vaccination for girls and women ages 13 through 26 who were never immunized. The CDC says it's ideal to get vaccinated before becoming sexually active, but vaccination after becoming sexually active can still offer protection because girls and women may not become exposed to all four HPV strains for many years. The vaccine doesn't treat existing infections, however.
The study published by researchers from the Harvard School of Public Health suggests Gardasil's cost is justified in pre-adolescent girls, partly because they are less likely to have already been exposed to HPV. But among older females, the cost-effectiveness of Gardasil becomes less and less favorable, researchers concluded. "Under most scenarios, extending the catchup to 26 wasn't cost-effective," Jane Kim, an assistant Harvard professor, said in an interview.
Merck, Whitehouse Station, N.J., disputed the conclusions, saying its own health-economic models suggest the vaccine is worth the cost. "We believe there's important value in vaccinating all women who are in the indicated age groups," said Rick Haupt, Merck's head of clinical research for Gardasil.
Ms. Kim and Harvard colleague Sue Goldie concluded that it cost about $43,600 per "quality-adjusted life year" gained, when HPV vaccine is administered to 12-year-old girls. This falls below the $50,000 per quality-adjusted life year threshold that some researchers use as a maximum for cost-effectiveness. Other researchers use a higher maximum benchmark of $100,000 per QALY to gauge cost-effectiveness.
It would cost $97,300 per QALY, however, to vaccinate girls and women through age 18, $120,400 per QALY for girls and women up to age 21, and $152,700 for girls and women up to age 26. The cost-effectiveness becomes more attractive when protection against genital warts is factored in.
The researchers arrived at these numbers by projecting HPV infection rates in various age groups, gauging the effectiveness of the vaccine and estimating cervical-cancer screening rates. Screening via Pap smear is recommended for women who are sexually active, even with the availability of Gardasil. The screenings can detect pre-cancerous lesions that can be removed; the availability of these tests has helped reduce the cervical-cancer death rate in the U.S. dramatically since the 1950s.
Merck's Dr. Haupt said the company's own models show that the cost per QALY is "well under $50,000" for women up to age 26. Among the differences between the models were that the Harvard researchers included patient time and travel costs, while Merck didn't, and the Harvard researchers didn't include genital warts in males, while Merck did, according to the CDC.
At least one of the factors in the primary Harvard calculations may be a relatively optimistic assumption -- that vaccination would produce lifelong immunity. Because the vaccine was only studied for five years and has been on the market for two years, no one knows for certain if its protection is lifelong, or if it wanes over time.
The Harvard researchers concluded that the cost per QALY would rise if the vaccine's effect wanes after 10 years.
Merck says the vaccine will offer protection well beyond five years, Dr. Haupt said. The Merck economic model that arrived at the cost per QALY below $50,000 assumed lifelong immunity, he said.
Still, the study is likely to fuel skepticism about Gardasil, which has already faced questions surrounding its safety and effectiveness (Merck and the CDC maintain it is safe and effective, with the most common side effect being soreness at site of injection.)
Labels: Cervical Cancer Vaccine, Gardasil

0 Comments:
Post a Comment
<< Home